The interpretation and effect of a low-carbohydrate diet in the management of type 2 diabetes: a systematic review and meta-analysis of randomised controlled trials
Abstract
Background/objectives
Recently, the role of a low-carbohydrate diet in diabetes management has generated interest with claims being made regarding its superiority over the traditional high-carbohydrate, low-fat dietary approach. This systematic review and meta-analysis evaluated the interpretation and effect of a low-carbohydrate diet in the management of type 2 diabetes.
Subjects/methods
Randomised controlled trials were searched for which included adults with type 2 diabetes aged 18 years or more. The intervention was a low-carbohydrate diet as defined by the author compared to a control group of usual care. MEDLINE, EMBASE, CINAHL, Cochrane Central Register of Controlled Trials, ISRCTN, ProQuest and opengrey.eu were searched. Independent experts were contacted and reference lists of selected papers were checked. Results were analysed descriptively and meta-analyses were completed to include trials that presented data at 1 year.
Results
Eighteen studies (n = 2204) were eligible for inclusion within the systematic review. The definition of a low-carbohydrate diet varied. At trial end, the descriptive analysis suggested that the low-carbohydrate intervention arm (LCIA) may promote favourable outcomes in terms of HbA1c, triglycerides and HDL cholesterol. The LCIA demonstrated reduced requirements for diabetes medication, which may have reduced the observed benefit of dietary carbohydrate restriction on HbA1c. Seven studies provided data to be included in the meta-analyses at 1 year. The meta-analyses showed statistical significance in favour of the LCIA for HbA1c (estimated effect = −0.28%, 95% CI −0.53 to −0.02, p = 0.03; χ2 = 13.15, df = 6, p = 0.03; I2 = 54%), HDL cholesterol (estimated effect = 0.06 mmol/L, 95% CI 0.04–0.09, p < 0.00001; χ2 = 6.05, df = 6, p = 0.42; I2 = 1%), triglycerides (estimated effect = −0.24 mmol/L, 95% CI −0.35 to −0.13, p < 0.0001; χ2 = 1.88, df = 6, p = 0.93; I2 = 0%) and systolic blood pressure (estimated effect = −2.74 mmHg, 95% CI −5.27 to −0.20, p = 0.03; χ2 = 10.54, df = 6, p = 0.10; I2 = 43%). Meta-analyses for weight, total cholesterol, LDL cholesterol and diastolic blood pressure did not demonstrate a statistically significant difference between interventions.
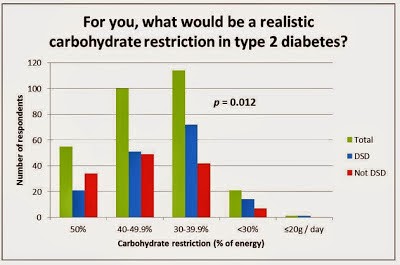
Dietary adherence was an issue in most studies. A very low-carbohydrate diet (<50 g/day) seems unrealistic in this population, however, a low-carbohydrate diet (<130 g/day) appears to be achievable. Improved clinical outcomes were observed in some studies as a result of achieving a low- or moderate-carbohydrate diet.
Fifteen out of 18 studies were considered high risk of bias, with performance bias being a common issue.
Conclusions
Reducing dietary carbohydrate may produce clinical improvements in the management of type 2 diabetes. Further research is needed to understand the true effect of dietary carbohydrate restriction on HbA1c independent of medication reduction and to address known issues with adherence to this dietary intervention. Clarity is needed regarding appropriate classification of a low-carbohydrate diet.
https://www.nature.com/articles/s41430-017-0019-4
Abstract
Background/objectives
Recently, the role of a low-carbohydrate diet in diabetes management has generated interest with claims being made regarding its superiority over the traditional high-carbohydrate, low-fat dietary approach. This systematic review and meta-analysis evaluated the interpretation and effect of a low-carbohydrate diet in the management of type 2 diabetes.
Subjects/methods
Randomised controlled trials were searched for which included adults with type 2 diabetes aged 18 years or more. The intervention was a low-carbohydrate diet as defined by the author compared to a control group of usual care. MEDLINE, EMBASE, CINAHL, Cochrane Central Register of Controlled Trials, ISRCTN, ProQuest and opengrey.eu were searched. Independent experts were contacted and reference lists of selected papers were checked. Results were analysed descriptively and meta-analyses were completed to include trials that presented data at 1 year.
Results
Eighteen studies (n = 2204) were eligible for inclusion within the systematic review. The definition of a low-carbohydrate diet varied. At trial end, the descriptive analysis suggested that the low-carbohydrate intervention arm (LCIA) may promote favourable outcomes in terms of HbA1c, triglycerides and HDL cholesterol. The LCIA demonstrated reduced requirements for diabetes medication, which may have reduced the observed benefit of dietary carbohydrate restriction on HbA1c. Seven studies provided data to be included in the meta-analyses at 1 year. The meta-analyses showed statistical significance in favour of the LCIA for HbA1c (estimated effect = −0.28%, 95% CI −0.53 to −0.02, p = 0.03; χ2 = 13.15, df = 6, p = 0.03; I2 = 54%), HDL cholesterol (estimated effect = 0.06 mmol/L, 95% CI 0.04–0.09, p < 0.00001; χ2 = 6.05, df = 6, p = 0.42; I2 = 1%), triglycerides (estimated effect = −0.24 mmol/L, 95% CI −0.35 to −0.13, p < 0.0001; χ2 = 1.88, df = 6, p = 0.93; I2 = 0%) and systolic blood pressure (estimated effect = −2.74 mmHg, 95% CI −5.27 to −0.20, p = 0.03; χ2 = 10.54, df = 6, p = 0.10; I2 = 43%). Meta-analyses for weight, total cholesterol, LDL cholesterol and diastolic blood pressure did not demonstrate a statistically significant difference between interventions.
Dietary adherence was an issue in most studies. A very low-carbohydrate diet (<50 g/day) seems unrealistic in this population, however, a low-carbohydrate diet (<130 g/day) appears to be achievable. Improved clinical outcomes were observed in some studies as a result of achieving a low- or moderate-carbohydrate diet.
Fifteen out of 18 studies were considered high risk of bias, with performance bias being a common issue.
Conclusions
Reducing dietary carbohydrate may produce clinical improvements in the management of type 2 diabetes. Further research is needed to understand the true effect of dietary carbohydrate restriction on HbA1c independent of medication reduction and to address known issues with adherence to this dietary intervention. Clarity is needed regarding appropriate classification of a low-carbohydrate diet.
https://www.nature.com/articles/s41430-017-0019-4